As federal health dollars disappear, L.A. County’s proposed tax hike may determine whether clinics stay open—or disparities deepen.
At first glance, the numbers don’t seem to add up. A half-cent sales tax increase—just 0.5 percent—hardly feels like a solution to billions of dollars in looming health-care cuts. But for Los Angeles County, officials say that tiny fraction may be the difference between a system that bends and one that breaks.
The stakes became clearer this month as two parallel funding crises collided.
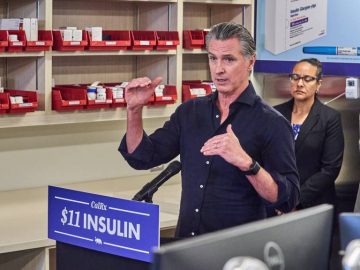
Between February 9 and 11, 2026, the U.S. Department of Health and Human Services announced plans to rescind roughly $600 million in CDC-administered public health grants from four Democratic-led states, with California absorbing nearly two-thirds of the cuts, according to HHS and state officials. The administration said the grants no longer align with “agency priorities,” targeting programs tied to HIV prevention, STI surveillance, data modernization, and public-health staffing.
Among the immediate impacts: Los Angeles County stands to lose more than $1 million for its National HIV Behavioral Surveillance Project alone, according to county health officials. California, Illinois, Colorado, and Minnesota filed suit on February 11, arguing the cuts are politically motivated and unlawful.
Yet those CDC grants—significant as they are—represent only a small slice of the fiscal shock hitting L.A. County.
The Bigger Threat: $2.4 Billion in Federal Losses
County leaders point to a far larger source of instability: the “One Big Beautiful Bill Act” (H.R. 1), a sweeping federal budget law passed in July 2025 that sharply reduces Medicaid and safety-net funding. Los Angeles County estimates it will lose $2.4 billion over three years, with funding cuts affecting 24 clinics, multiple county hospitals, and contributing to more than 120,000 residents losing Medi-Cal coverage so far.
Against that backdrop, on February 10, the L.A. County Board of Supervisors voted 4–1 to place a temporary half-cent sales tax increase on the June 2026 ballot. The measure—called the Essential Services Restoration Act—would raise the county’s base sales tax from 9.75% to 10.25% for five years, generating an estimated $1 billion annually.
Supervisors Holly Mitchell and Hilda Solis, who sponsored the measure, framed it as a stopgap—not an expansion, but a way to keep emergency rooms open, clinics staffed, and care accessible.
Why 0.5% Matters
For an individual shopper, the increase amounts to pennies on everyday purchases. For the county’s health system, officials say it could stabilize trauma centers, preserve public-health jobs, and prevent deeper service cuts—especially in communities already facing barriers to care.
Opponents, including Supervisor Kathryn Barger and the Howard Jarvis Taxpayers Association, argue residents shouldn’t be asked to “backfill” federal decisions and warn about affordability.
But county health leaders counter that the cost of doing nothing is far higher—measured not just in dollars, but in delayed care, shuttered clinics, and preventable illness.
Our community is always the hardest hit
For Latino families, where uninsurance and barriers to preventive care remain stubbornly high, the timing could not be worse. According to federal health data, Latinos have the highest uninsured rate of any major racial/ethnic group—approximately 17% lack coverage, more than double the overall U.S. rate—leaving many at risk of delayed detection and treatment for chronic illness. Source OMH
Latino adults also experience disproportional burdens from leading killers such as heart disease, diabetes, and cancer, risks that are amplified by limited access to routine care and preventive services. Recent analyses found Latinos continue to face obstacles to care—such as delayed treatment due to cost or lack of insurance—despite progress in coverage expansion.
In a budget measured in tens of billions, half a cent won’t fix everything. But in a moment of cascading federal withdrawals, L.A. County officials argue it could buy something increasingly rare in public health: time—and stability—when communities need it most.